By María José Patiño Valiente. *
Chronic non-communicable diseases (CNCDs) are one of the leading annual causes of global deaths. Statistics from the World Health Organization (WHO) show CNCD related deaths have increased by 28% worldwide. The Global Burden of Disease (GBD) Study points out that youth and middle-aged adults suffer most from CNCDs. Globally, 40% of these diseases occurred in people under 70 years of age and 87% of premature deaths occurred in low- to middle-income countries. Unfortunately, the COVID-19 pandemic has hurt the advances that countries had been making in slowing down the progress of CNCDs, while also impacting health care shortcomings. Many patients suffering from one or more CNCDs have had to cancel or postpone treatment, resulting in increasing deaths from these diseases. Unfortunately, patients living with one or more NCDs are also more vulnerable to COVID-19 infection or death.
The prevalence of NCDs is the result of a complex interaction between public health and a country´s economic growth and development. The diseases are strongly associated with trends such as population aging, accelerated and unplanned urbanization, and the globalization of unhealthy lifestyles. This results in decreased productivity, prolonged disability, and strains on family economic resources, since in many cases people must use their own means to finance medical treatments. As a result, there are excessive out-of-pocket expenses, in some cases catastrophic, which further impoverishes the population, given the failing health system in many countries.
Data from the WHO allow a regional analysis of countries grouped by income level (low-income countries, low-to-middle-income countries, middle-to-high-income countries, high-income countries). In this analysis, 77% of all deaths from NCDs occur in low- to middle-income countries. Young and working-age populations are the most affected by CNCDs in these countries, thus perpetuating the fragile conditions of their quality of life.
Saving and prolonging the life of a patient is the responsibility of the country’s health system. The mitigation and prevention of contracting these diseases should be a priority for those designing public policies. Public health improvements are the comprehensive result of the country´s sustainable economic growth and development along with better education and optimal urban development.
Thus, the severity of these diseases stems from the loss of life and patients’. In addition, these CNCDs have a macroeconomic effect due to the excessive health spending (private and public) to treat them as well as from productivity losses that cause irrecoverable damage to the country’s economy. The World Economic Forum (WEF) mentions in its report that the global economic burden of the treatment of CNCDs is around 30 trillion dollars, representing approximately 48% of global GDP. In turn, Deloitte points out that current global health expenditures are approximately 8.7 trillion dollars, of which 50% is earmarked for the treatment of these diseases. The amounts related to these diseases are remarkably high and it is urgent to reduce their prevalence in the global population.
As a result, the WHO and the WEF propose a set of intervention strategies, known as “best-buys for CNCDs”, in order to reduce the spread of these diseases in the population. Interventions from counseling and drug therapy for cardiovascular diseases to measures to prevent cervical cancer are estimated to require an investment of between US $ 1 to US $ 3 per person, depending on whether the country is low- or middle-income. The returns on this investment would prevent millions of premature deaths and generate millions of dollars of additional production. The WHO’s efforts are expected to help countries continue to reduce the prevalence of these diseases in their populations.
Suffering from one or more CNCDs would be disastrous, regardless of whether the patient lives in a country with high, medium or low income and whether or not they have universal health coverage. Results would probably be most optimal for treatments available in rich countries compared to poor countries; however, the negative consequences affect everyone. Saving and prolonging the life of a patient is the responsibility of the country’s health system. The mitigation and prevention of contracting these diseases should be a priority for those designing public policies. Public health improvements are the comprehensive result of the country´s sustainable economic growth and development along with better education and optimal urban development. In addition, the current crisis unleashed by COVID-19 presents an opportunity for countries to learn key lessons and redesign their public health strategies in order to provide better health services for their populations.
* María José Patiño Valiente is an economist, graduated with honors from the National University of Asunción, Paraguay, and has a master’s degree in Agribusiness and Agricultural Economics from the University of Manitoba, Canada. She has more than 10 years of experience working for government institutions, academia and the private sector. She is currently working as an International Consultant for different companies, especially in the agri-food sector.
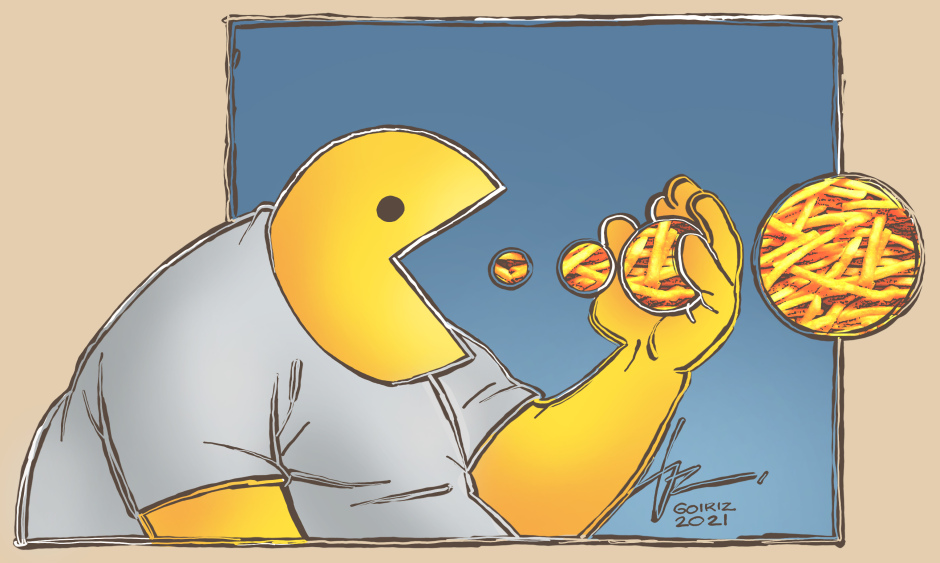
Illustration: Roberto Goiriz
